43 year old male with bilateral loin pain and pain abdomen
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box is welcome.
Here is a case i have seen:
A 43 year old male presented with C/o vomitings,decreased appetite, b/l loin pain since 12 days
Pt was apparently asymptomatic 12 days back then he c/o decreased appetite since 12 days and vomitings immediately after intake of solids, liquids which was non bilious,non blood stained since 12 days and stopped 4d ys back
C/o burning micturition since 12 days
C/o decreased urine output since 10 days, c/o constipation since 10 days, fever since 4 days(subsided now)
No history of pedal edema, cough,cold,sob,palpitation
Pt had h/o similar complaints in the past ?pancreatitis 7 years back
Pt had h/o usage of NSAIDS for?joint pains since 7 years
8 yrs back h/o skid and fall from bike and sustained trauma to RT knee for which casting was done
Since 7 yrs b/l knee pain started , on and off after 6 months generalized joint pains , non radiating , on and off ( b/l wrist , elbow , shoulder , ankle , small joints of fingers for which he took multiple injections of tramadol , decadron )
There is no h /o morning stiffness , fever
In the past 6 months he didn't took any injections , he was using tablet pcm whenever he has pain .
H/o of swelling present since 7 yrs at b/l metatarsophalangeal joints , elbow , sternoclavicular joint . He developed b/l knee swelling 5 yrs back for which pus was aspirated ( each knee joint 2 times ) and took some antibiotic injections ( no records available )
K/c/o chronic alcoholic since 20 years daily 90ml
Not a smoker
Not a k/c/o DM, HTN, CVA, CAD, epilepsy, asthma
Examination :
O/e pt is c/c/c
Afebrile to touch
PR:80bpm
BP:120/70
Spo2:98
P/A:soft,tenderness present on b/l loin region, rt hypochondrium, hepatospenomegaly present,BS:sluggish
RS:B/LAE+,nvbs
CVS:s1,s2+,no murmurs
CNS:no FND
Investigations at admission
Day 2
C/o B/L loin pain decreasing in intensity
C/o constipation since 19days,not passing flatus
No fever spikes over night
Grbs 191
I/0 1500/1800
Ryles drain 100ml
O/e pt is c/c/c
Afebrile to touch
PR:80bpm
BP:130/90
Spo2:80
P/A:soft,tenderness present on b/l loin region, rt hypochondrium, hepatospenomegaly present,BS:sluggish RS:B/LAE+,nvbs
CVS:s1,s2+,no murmurs , CNS - no FND
Treatment sips of water plus same treatment
Day 3
C/o b/l loin pain decreasing intensity
C/o constipation since 12 days , passing flatus
No fever spikes
Grbs - 181
I/O - 2100/2300
Ryles drain - 500ml
O/e :
Pt is c/c/c
Pr - 78bpm , regular BP -120/80mmhg
CVS - S1 S2 + , RS - BAE + NVBS , CNS - no FND
P/A - tenderness in RT hypochondrium
B/l loin pain . BS sluggish
Treatment
Plenty of oral fluids - 3l/ day , liquid diet
Plus same treatment given
Rules tube removed
Soap water enema at 8pm
Day 4
Passed stools yesterday night
No fever spikes
GRBS - 187
I/O - 2250/2300
O/e :
Pt is c/c/c
PR - 72bpm regular BP - 110/70 mmHg
CVS - S1 S2+ ,. RS - BAE + NVBS , CNS - no FND
P/A - soft, tenderness in RT hypochondrium
BS + sluggish
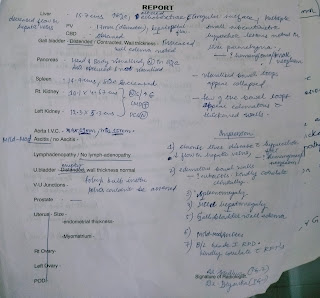
Diagnosis : Acute pyelonephr itis, Chronic pancreatitis , Pre renal Aki ( resolving ) , soft tissue mass in mesentery ? Malignancy , alcohol dependence syndrome.





























Comments
Post a Comment